The Future of US Healthcare: Shaping the Landscape of 2025
Related Articles: The Future of US Healthcare: Shaping the Landscape of 2025
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to The Future of US Healthcare: Shaping the Landscape of 2025. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
- 1 Related Articles: The Future of US Healthcare: Shaping the Landscape of 2025
- 2 Introduction
- 3 The Future of US Healthcare: Shaping the Landscape of 2025
- 4 Related Searches
- 5 FAQs by Trends in US Healthcare 2025
- 6 Tips by Trends in US Healthcare 2025
- 7 Conclusion by Trends in US Healthcare 2025
- 8 Closure
The Future of US Healthcare: Shaping the Landscape of 2025

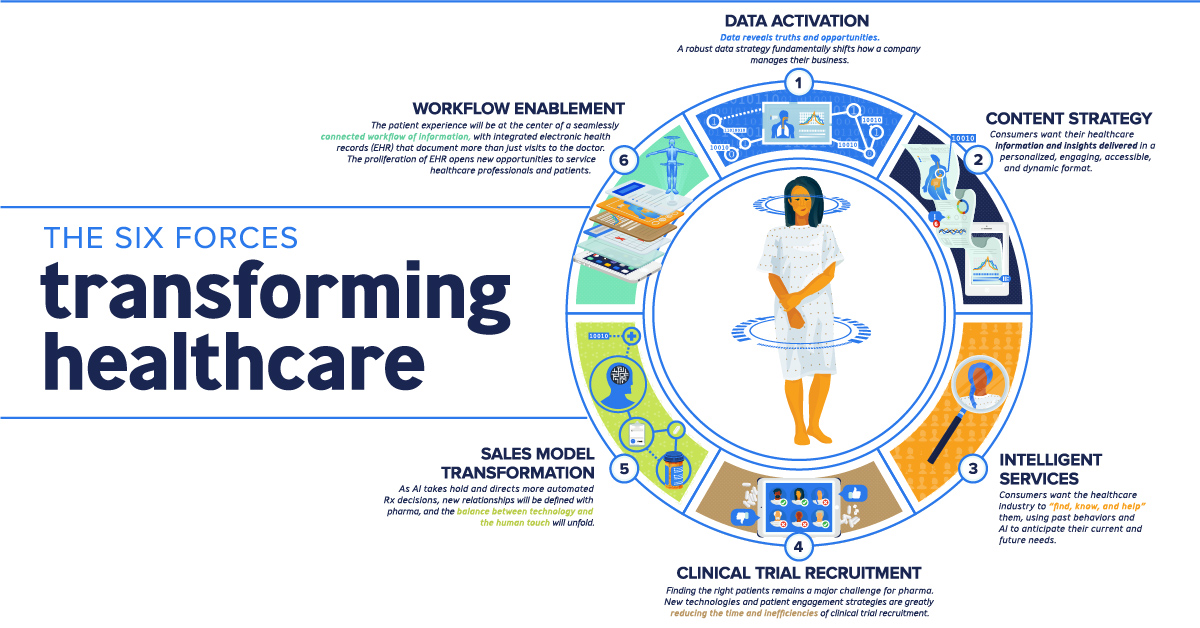
The US healthcare system is in a constant state of evolution, driven by technological advancements, shifting demographics, and a growing emphasis on value-based care. As we approach 2025, several key trends are poised to reshape the landscape of healthcare delivery, access, and cost. Understanding these trends is crucial for patients, providers, and policymakers alike, as they will influence the future of health and well-being for millions of Americans.
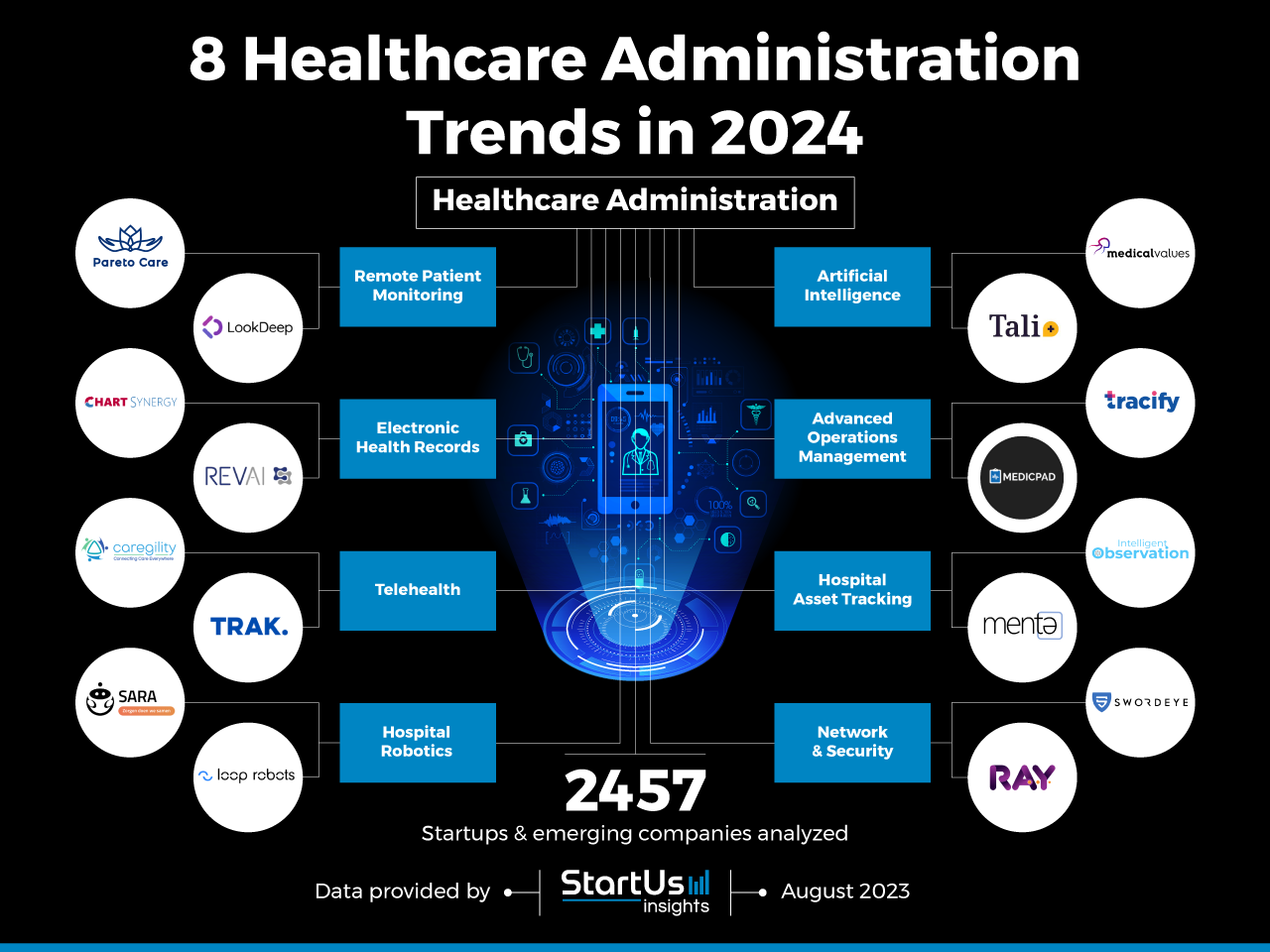
1. The Rise of Virtual Care and Telemedicine
The COVID-19 pandemic accelerated the adoption of virtual care, and this trend shows no signs of slowing down. Telemedicine, remote patient monitoring, and telehealth platforms are becoming increasingly integrated into the healthcare ecosystem, offering patients greater convenience, accessibility, and affordability.
Benefits:
- Enhanced Access: Telemedicine eliminates geographical barriers, enabling patients in rural areas or with limited mobility to access specialized care.
- Reduced Costs: Virtual consultations and remote monitoring can reduce travel expenses, waiting times, and overall healthcare costs.
- Improved Patient Engagement: Telehealth platforms facilitate communication and collaboration between patients and providers, leading to better adherence to treatment plans and improved health outcomes.
Challenges:
- Privacy and Security: Ensuring the confidentiality and security of patient data in a virtual environment is paramount.
- Reimbursement Policies: Clear and consistent reimbursement policies for telehealth services are needed to ensure provider sustainability.
- Digital Divide: Addressing the digital divide and ensuring equitable access to virtual care for all patients is essential.
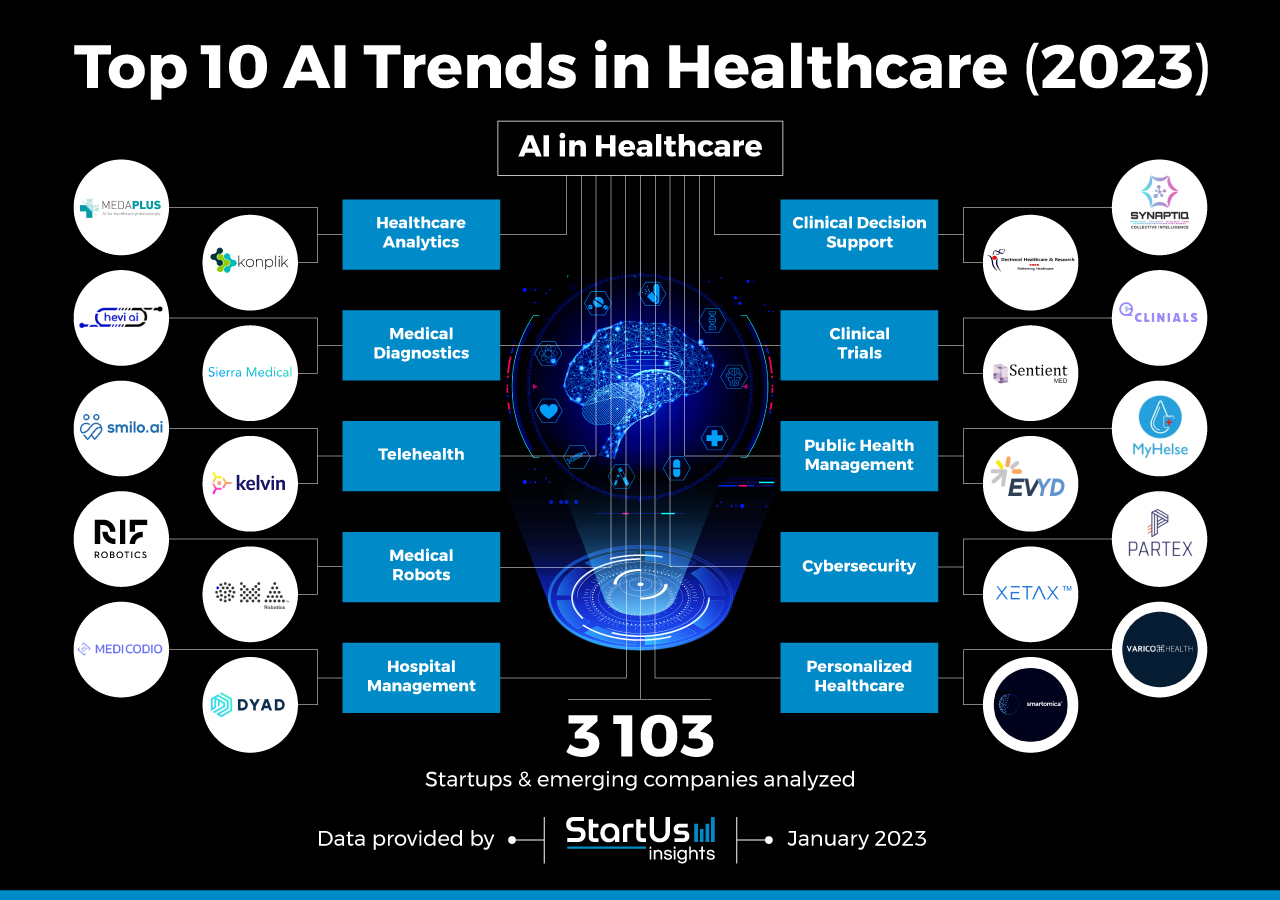
2. The Integration of Artificial Intelligence (AI) and Machine Learning (ML)
AI and ML are rapidly transforming healthcare, enabling faster and more accurate diagnoses, personalized treatment plans, and more efficient administrative processes. These technologies are being leveraged in areas such as:
- Image Analysis: AI-powered tools can assist radiologists in detecting and diagnosing diseases from medical images.
- Drug Discovery: ML algorithms can accelerate the process of developing new drugs and therapies.
- Predictive Analytics: AI can help identify patients at risk of developing certain conditions, allowing for proactive interventions.
Benefits:
- Improved Accuracy and Efficiency: AI can enhance the speed and accuracy of diagnoses and treatment decisions.
- Personalized Medicine: AI-powered tools enable the development of tailored treatment plans based on individual patient characteristics.
- Enhanced Operational Efficiency: AI can automate administrative tasks, freeing up clinicians’ time for patient care.
Challenges:
- Data Privacy and Bias: Ensuring the ethical use of AI and ML algorithms, addressing potential biases, and safeguarding patient privacy is crucial.
- Transparency and Explainability: Understanding how AI algorithms make decisions and ensuring transparency in their operation is essential for patient trust.
- Job Displacement: The potential for AI to automate certain tasks raises concerns about job displacement in the healthcare industry.
3. The Focus on Value-Based Care
Value-based care models incentivize providers to deliver high-quality care while managing costs effectively. This shift from fee-for-service models emphasizes outcomes and patient satisfaction, leading to:
- Population Health Management: Providers are increasingly responsible for managing the health of entire patient populations, focusing on preventive care and disease management.
- Care Coordination: Seamless coordination of care among different providers and settings is crucial for achieving optimal patient outcomes.
- Patient Engagement: Empowering patients to actively participate in their care through tools like patient portals and mobile apps is essential.
Benefits:
- Improved Health Outcomes: By focusing on prevention and early intervention, value-based care aims to improve patient health and well-being.
- Reduced Healthcare Costs: By optimizing resource allocation and promoting efficient care delivery, value-based care can help control rising healthcare costs.
- Enhanced Patient Satisfaction: A patient-centered approach leads to improved communication, trust, and satisfaction with the healthcare experience.
Challenges:
- Data Collection and Analytics: Implementing value-based care requires robust data collection and analysis capabilities to measure outcomes and identify areas for improvement.
- Provider Incentives: Aligning provider incentives with value-based care principles is essential to ensure their engagement and commitment.
- Interoperability: Seamless data sharing and communication between different healthcare providers and systems is crucial for effective care coordination.
4. The Growing Importance of Behavioral Health
The integration of behavioral health into primary care settings is becoming increasingly recognized as essential for holistic patient well-being. This trend addresses the growing prevalence of mental health conditions and the need for comprehensive care:
- Integrated Care Models: Primary care providers are increasingly equipped to screen for and manage common mental health conditions, offering patients access to integrated care.
- Mental Health Professionals in Primary Care: Collaboration between primary care physicians and mental health professionals ensures coordinated care and reduces stigma associated with mental health services.
- Teletherapy and Digital Mental Health Tools: Virtual platforms and digital tools are expanding access to behavioral health services, offering convenient and affordable options for patients.
Benefits:
- Early Detection and Intervention: Integrating behavioral health into primary care settings enables earlier detection and intervention for mental health conditions, improving patient outcomes.
- Reduced Stigma: Breaking down silos between physical and mental health care reduces stigma and encourages patients to seek help.
- Improved Overall Health: Addressing mental health needs alongside physical health concerns leads to better overall health and well-being.
Challenges:
- Reimbursement Policies: Ensuring adequate reimbursement for behavioral health services is crucial for provider sustainability.
- Mental Health Workforce Shortage: Addressing the shortage of mental health professionals is essential to meet growing demand.
- Cultural Sensitivity: Providing culturally sensitive and equitable behavioral health services is essential for all patients.
5. The Rise of Consumerism in Healthcare
Patients are becoming increasingly empowered consumers, demanding greater transparency, control, and personalized care. This trend is driving innovation in healthcare, with:
- Patient Portals and Mobile Apps: Patients are using online platforms and mobile apps to access their medical records, schedule appointments, and manage their health information.
- Direct-to-Consumer Healthcare Services: Companies are offering direct-to-consumer services like genetic testing, virtual consultations, and personalized health plans.
- Price Transparency: Patients are demanding more information about healthcare costs, leading to increased transparency and price comparisons.
Benefits:
- Enhanced Patient Engagement: Consumers are taking a more active role in their health, leading to better adherence to treatment plans and improved outcomes.
- Increased Choice and Control: Patients have greater access to information and options, enabling them to make informed decisions about their care.
- Innovation and Competition: Consumerism is driving innovation and competition in the healthcare industry, leading to better services and lower costs.
Challenges:
- Data Privacy and Security: Protecting patient data in a consumer-driven environment is crucial.
- Quality and Safety: Ensuring the quality and safety of direct-to-consumer healthcare services is essential.
- Health Literacy: Addressing health literacy disparities and empowering all patients to navigate the complex healthcare system is critical.
6. The Growing Importance of Data Analytics and Interoperability
The increasing volume and complexity of healthcare data require sophisticated analytics tools and interoperable systems to extract meaningful insights and improve decision-making. This trend is driving:
- Data Warehousing and Analytics: Healthcare organizations are investing in data warehousing and analytics platforms to collect, store, and analyze vast amounts of patient data.
- Health Information Exchanges (HIEs): HIEs facilitate secure data sharing between different healthcare providers and systems, improving care coordination and patient safety.
- Precision Medicine: Data analytics enables the development of personalized treatment plans based on individual patient characteristics and genetic information.
Benefits:
- Improved Patient Care: Data-driven insights can help identify patients at risk, predict health outcomes, and personalize treatment plans.
- Enhanced Efficiency and Cost Savings: Data analytics can optimize resource allocation, streamline workflows, and reduce unnecessary costs.
- Research and Innovation: Access to large datasets fuels research and innovation in healthcare, leading to new discoveries and treatments.
Challenges:
- Data Security and Privacy: Protecting sensitive patient data is paramount in a data-driven healthcare environment.
- Interoperability Standards: Establishing consistent and standardized data exchange protocols is essential for seamless data sharing.
- Data Governance and Ethics: Ensuring the responsible use of healthcare data, addressing ethical concerns, and protecting patient privacy is crucial.
7. The Focus on Workforce Development and Diversity
The healthcare workforce is facing a growing demand for skilled professionals, particularly in areas like telehealth, data analytics, and behavioral health. Addressing workforce shortages and promoting diversity is crucial for:
- Training and Education: Investing in training programs and educational initiatives to develop a skilled healthcare workforce is essential.
- Diversity and Inclusion: Creating a more diverse and inclusive healthcare workforce that reflects the patient population is crucial for providing equitable care.
- Addressing Workforce Shortages: Implementing strategies to attract and retain healthcare professionals, particularly in rural and underserved areas, is essential.
Benefits:
- Improved Patient Care: A skilled and diverse workforce can provide better care to a wider range of patients.
- Enhanced Innovation: A diverse workforce brings new perspectives and ideas, fostering innovation and creativity in healthcare.
- Increased Access to Care: Addressing workforce shortages and expanding the healthcare workforce can improve access to care for all patients.
Challenges:
- Training and Education Costs: Investing in workforce development requires significant financial resources.
- Attracting and Retaining Talent: Competing for talent in a tight labor market can be challenging.
- Addressing Workforce Shortages in Underserved Areas: Attracting and retaining healthcare professionals in rural and underserved areas requires specific incentives and strategies.
8. The Impact of Climate Change on Healthcare
Climate change is increasingly recognized as a significant threat to public health, impacting the incidence of certain diseases, exacerbating existing health conditions, and leading to increased healthcare costs.
- Heat-Related Illnesses: Extreme heat events can lead to heat stroke, dehydration, and other heat-related illnesses.
- Air Pollution: Air pollution from wildfires, industrial emissions, and other sources can exacerbate respiratory conditions and contribute to cardiovascular disease.
- Infectious Diseases: Changing environmental conditions can affect the spread of infectious diseases like malaria and dengue fever.
Benefits:
- Early Prevention and Mitigation: Addressing climate change through mitigation and adaptation strategies can reduce the impact on public health.
- Sustainable Healthcare Systems: Transitioning to more sustainable healthcare practices can reduce the industry’s carbon footprint.
Challenges:
- Addressing Climate Change Impacts: Developing effective strategies to mitigate and adapt to the health impacts of climate change is crucial.
- Investing in Climate-Resilient Healthcare Systems: Building climate-resilient healthcare infrastructure and systems is essential to ensure access to care during extreme weather events.
- Public Health Education and Awareness: Raising public awareness about the health impacts of climate change and promoting healthy behaviors is critical.
Related Searches
1. Healthcare Technology Trends 2025: This search focuses on the technological advancements shaping the future of healthcare, including AI, telemedicine, and wearable technology.
2. Future of Healthcare in the US: This broader search explores the long-term trends and challenges facing the US healthcare system, including cost containment, access to care, and population health management.
3. Healthcare Innovation Trends: This search focuses on the innovative solutions and breakthroughs emerging in healthcare, including new drug development, personalized medicine, and gene editing.
4. Healthcare Industry Trends 2025: This search examines the overall trends affecting the healthcare industry, including mergers and acquisitions, regulatory changes, and the evolving role of payers and providers.
5. Healthcare Policy Trends: This search explores the policy changes and initiatives shaping the future of healthcare, including Medicare and Medicaid reform, drug pricing, and value-based care models.
6. Healthcare Workforce Trends: This search focuses on the challenges and opportunities facing the healthcare workforce, including workforce shortages, diversity and inclusion, and the impact of technology on job roles.
7. Healthcare Costs Trends: This search examines the rising costs of healthcare and the factors contributing to them, including aging populations, technological advancements, and prescription drug prices.
8. Healthcare Consumerism Trends: This search explores the growing influence of consumers on healthcare decisions, including the demand for transparency, personalization, and convenient access to care.
FAQs by Trends in US Healthcare 2025
1. What are the main benefits of virtual care and telemedicine?
Virtual care and telemedicine offer several benefits, including:
- Enhanced access to care: Patients in rural areas or with limited mobility can access specialized care remotely.
- Reduced costs: Virtual consultations and remote monitoring can reduce travel expenses, waiting times, and overall healthcare costs.
- Improved patient engagement: Telehealth platforms facilitate communication and collaboration between patients and providers, leading to better adherence to treatment plans and improved health outcomes.
2. How is AI being used in healthcare?
AI is being used in various ways in healthcare, including:
- Image analysis: AI-powered tools can assist radiologists in detecting and diagnosing diseases from medical images.
- Drug discovery: ML algorithms can accelerate the process of developing new drugs and therapies.
- Predictive analytics: AI can help identify patients at risk of developing certain conditions, allowing for proactive interventions.
3. What are the key principles of value-based care?
Value-based care models emphasize:
- High-quality care: Providers are incentivized to deliver high-quality care that meets patient needs.
- Cost-effectiveness: Providers are encouraged to manage costs effectively while maintaining quality.
- Patient outcomes: Value-based care focuses on improving patient health outcomes and satisfaction.
4. How is behavioral health being integrated into primary care?
Integrated care models are being implemented to:
- Screen for and manage mental health conditions: Primary care providers are increasingly equipped to screen for and manage common mental health conditions.
- Collaborate with mental health professionals: Collaboration between primary care physicians and mental health professionals ensures coordinated care.
- Expand access to behavioral health services: Teletherapy and digital tools are expanding access to behavioral health services.
5. What are the implications of consumerism in healthcare?
Consumerism is driving:
- Greater transparency and control: Patients are demanding more information about healthcare costs and options.
- Personalized care: Patients are expecting tailored treatment plans and services.
- Innovation and competition: Consumer demand is driving innovation and competition in the healthcare industry.
6. How can data analytics improve healthcare?
Data analytics can:
- Identify patients at risk: Data-driven insights can help identify patients at risk of developing certain conditions.
- Predict health outcomes: Analytics can help predict patient outcomes and personalize treatment plans.
- Optimize resource allocation: Data analytics can streamline workflows and reduce unnecessary costs.
7. What are the challenges of addressing workforce shortages in healthcare?
Addressing workforce shortages requires:
- Investing in training and education: Developing a skilled healthcare workforce requires significant financial resources.
- Attracting and retaining talent: Competing for talent in a tight labor market can be challenging.
- Addressing workforce shortages in underserved areas: Attracting and retaining healthcare professionals in rural and underserved areas requires specific incentives and strategies.
8. How does climate change impact healthcare?
Climate change can:
- Increase the incidence of heat-related illnesses: Extreme heat events can lead to heat stroke and other heat-related illnesses.
- Exacerbate existing health conditions: Air pollution and other environmental factors can worsen respiratory and cardiovascular conditions.
- Increase healthcare costs: The health impacts of climate change can lead to higher healthcare expenditures.
Tips by Trends in US Healthcare 2025
- Embrace virtual care: Patients and providers should embrace the convenience and accessibility of virtual care, leveraging telehealth platforms and remote monitoring tools.
- Stay informed about AI advancements: Healthcare professionals and patients should stay informed about the latest developments in AI and ML, understanding their potential benefits and challenges.
- Engage in value-based care models: Providers should actively participate in value-based care initiatives, focusing on improving patient outcomes and managing costs effectively.
- Prioritize behavioral health integration: Primary care providers should prioritize the integration of behavioral health services, addressing the growing need for mental health care.
- Advocate for consumer-driven healthcare: Patients should advocate for greater transparency, control, and personalized care in the healthcare system.
- Leverage data analytics for better decision-making: Healthcare organizations should invest in data warehousing and analytics platforms to extract meaningful insights and improve patient care.
- Support workforce development and diversity: Policymakers and healthcare organizations should invest in training programs and initiatives to develop a skilled and diverse healthcare workforce.
- Address the health impacts of climate change: Healthcare professionals and policymakers should prioritize strategies to mitigate and adapt to the health impacts of climate change.
Conclusion by Trends in US Healthcare 2025
The US healthcare system is poised for significant transformation in the years leading up to 2025. The trends outlined in this article will continue to shape the landscape of healthcare delivery, access, and cost, influencing the health and well-being of millions of Americans. By embracing these trends, leveraging technological advancements, and prioritizing patient-centered care, the US healthcare system can navigate the challenges and opportunities of the future, ensuring a healthier and more equitable healthcare experience for all.



Closure
Thus, we hope this article has provided valuable insights into The Future of US Healthcare: Shaping the Landscape of 2025. We appreciate your attention to our article. See you in our next article!