Anesthesia for Cataract Surgery: Recent Trends 2025
Related Articles: Anesthesia for Cataract Surgery: Recent Trends 2025
Introduction
With great pleasure, we will explore the intriguing topic related to Anesthesia for Cataract Surgery: Recent Trends 2025. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
- 1 Related Articles: Anesthesia for Cataract Surgery: Recent Trends 2025
- 2 Introduction
- 3 Anesthesia for Cataract Surgery: Recent Trends 2025
- 3.1 Understanding the Evolution of Anesthesia for Cataract Surgery
- 3.2 Recent Trends Shaping Anesthesia for Cataract Surgery in 2025
- 3.3 Related Searches
- 3.4 FAQs
- 3.5 Tips for Choosing the Right Anesthesia for Cataract Surgery
- 3.6 Conclusion
- 4 Closure
Anesthesia for Cataract Surgery: Recent Trends 2025
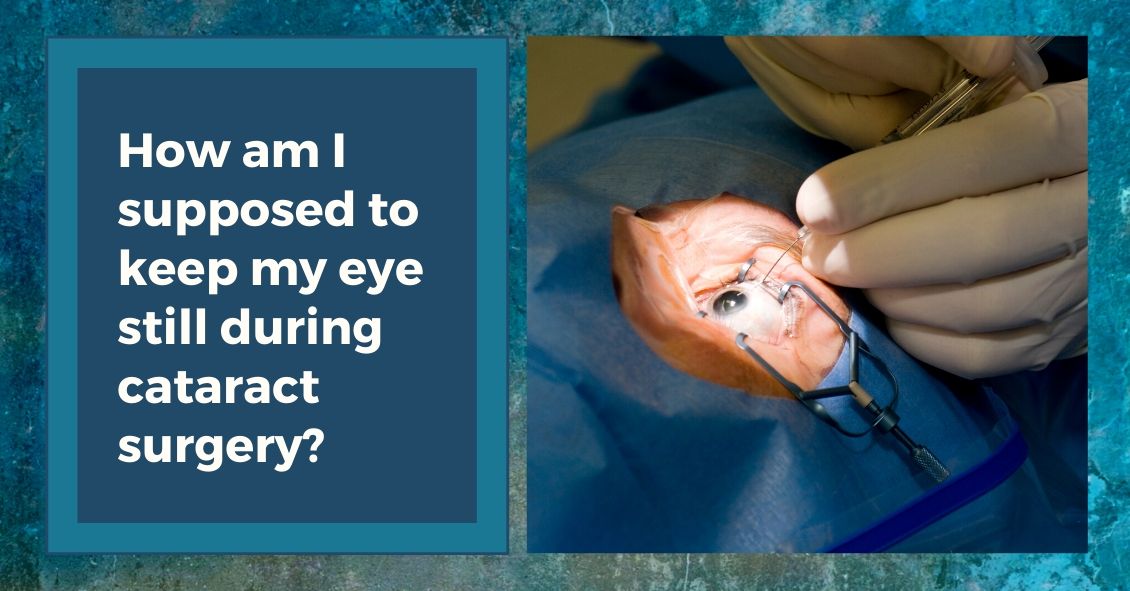
Cataract surgery is a remarkably safe and effective procedure, restoring vision for millions worldwide. However, the anesthetic approach plays a crucial role in ensuring patient comfort and a smooth surgical experience. The field of anesthesia is constantly evolving, and anesthesia for cataract surgery is no exception. This article explores the latest trends shaping anesthetic practices for this common procedure, looking ahead to 2025 and beyond.
Understanding the Evolution of Anesthesia for Cataract Surgery
Traditionally, cataract surgery was performed under general anesthesia, requiring patients to be completely unconscious. However, advances in ophthalmic techniques and patient preferences have led to a shift towards regional anesthesia, specifically topical anesthesia and peribulbar blocks. This evolution has brought about significant benefits, including:
- Reduced risk of complications: General anesthesia carries a higher risk of complications, especially in older patients, who are more likely to have underlying health conditions.
- Faster recovery: Patients recovering from regional anesthesia typically experience a quicker return to normal activity.
- Improved patient satisfaction: Many patients prefer the convenience and control offered by regional anesthesia, avoiding the need for intubation and a prolonged recovery period.
Recent Trends Shaping Anesthesia for Cataract Surgery in 2025
Several key trends are poised to further refine anesthetic practices for cataract surgery in the coming years:
1. Personalized Anesthesia:
The era of one-size-fits-all anesthesia is fading. With an increasing understanding of individual patient needs and risk factors, a personalized approach to anesthesia is gaining traction. This entails:
- Preoperative assessment: Thorough evaluation of patients’ medical history, medications, and allergies is essential to tailor anesthesia to their specific needs.
- Patient education: Open communication and informed consent are crucial, empowering patients to actively participate in their anesthetic care.
- Tailored anesthetic techniques: Choosing the most suitable anesthetic technique based on patient factors, such as age, medical history, and surgical complexity, ensures optimal comfort and safety.
2. Enhanced Topical Anesthesia:
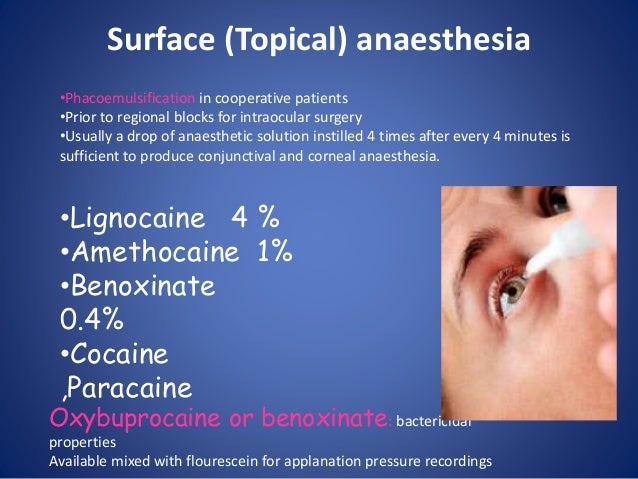
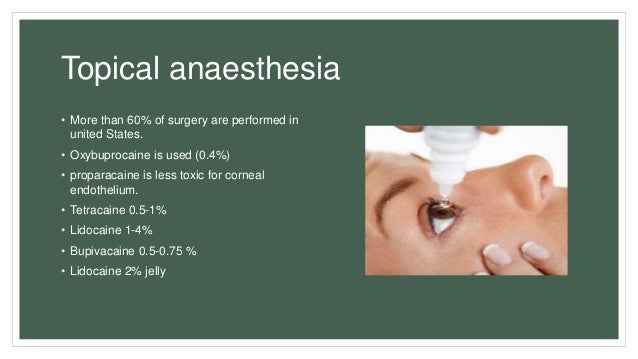
Topical anesthesia, involving the application of anesthetic drops to the eye, has become a mainstay in cataract surgery. However, ongoing research is focusing on:
- Improved formulations: Developing more potent and longer-lasting topical anesthetic agents reduces discomfort during the procedure.
- Combination therapies: Combining topical anesthetics with other agents, such as vasoconstrictors, can enhance effectiveness and minimize side effects.
- Targeted delivery: Novel drug delivery systems, such as micro-needles, may offer more precise and targeted anesthetic delivery.
3. Minimally Invasive Anesthesia Techniques:
Minimally invasive anesthesia techniques are gaining popularity, aiming to reduce pain and discomfort while maintaining safety and effectiveness. These include:
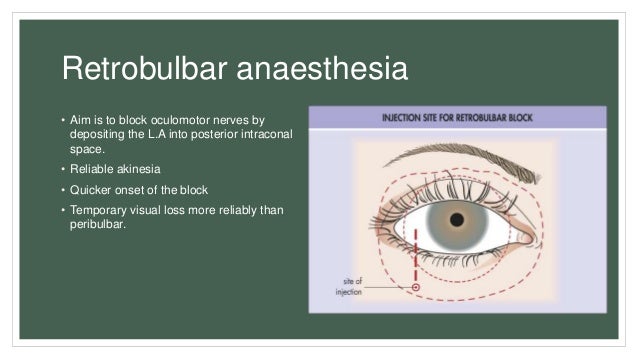
- Peribulbar blocks with ultrasound guidance: Ultrasound guidance allows for more precise anesthetic delivery, minimizing the risk of complications and enhancing patient comfort.
- Subconjunctival blocks: Injecting anesthetic directly into the space beneath the conjunctiva, the clear membrane covering the white part of the eye, provides effective pain relief with minimal side effects.
- Intravenous sedation: For patients who require additional sedation, intravenous sedation can be administered alongside regional anesthesia, providing a comfortable and relaxing experience.
4. Integration of Technology:
Technology is playing an increasingly important role in optimizing anesthetic care for cataract surgery:
- Automated drug delivery systems: Automated systems ensure accurate and consistent drug administration, improving safety and efficiency.
- Real-time monitoring: Continuous monitoring of vital signs, such as heart rate, blood pressure, and oxygen saturation, allows for prompt identification and management of potential complications.
- Artificial intelligence (AI): AI algorithms can analyze patient data and predict anesthetic requirements, potentially leading to more personalized and effective anesthetic care.
5. Focus on Patient Experience:
Improving the patient experience is a key priority in modern anesthesia. This involves:
- Preoperative counseling: Providing comprehensive information about anesthesia options, potential risks and benefits, and expected recovery allows patients to make informed decisions.
- Comfort and relaxation techniques: Implementing techniques such as music therapy, aromatherapy, and guided imagery can help patients feel more relaxed and comfortable during the procedure.
- Postoperative pain management: Proactive pain management strategies, including medications and non-pharmacological interventions, ensure a smooth and comfortable recovery.
Related Searches
Anesthesia for Cataract Surgery is a broad topic with several related searches, each offering valuable insights into specific aspects of this field. Here’s a closer look at some of the most common related searches:
1. Types of Anesthesia for Cataract Surgery:
This search explores the different anesthetic options available for cataract surgery, including:
- General Anesthesia: This involves complete unconsciousness, often used for complex surgeries or patients with specific medical conditions.
- Regional Anesthesia: This focuses on numbing a specific area of the body, typically the eye, using techniques like topical anesthesia, peribulbar blocks, and retrobulbar blocks.
- Sedation: This involves a state of relaxation and drowsiness, often used in conjunction with regional anesthesia.
2. Risks of Anesthesia for Cataract Surgery:
This search focuses on the potential risks associated with different anesthetic techniques, including:
- General anesthesia: Risks include respiratory complications, allergic reactions, and postoperative nausea and vomiting.
- Regional anesthesia: Risks include bleeding, nerve damage, and infection.
- Topical anesthesia: Risks include eye irritation, allergic reactions, and temporary blurred vision.
3. Anesthesia for Cataract Surgery in Children:
This search addresses the unique considerations for administering anesthesia to children undergoing cataract surgery, including:
- Choosing the appropriate anesthetic technique: General anesthesia is often preferred for children, as it ensures their complete immobility and cooperation during surgery.
- Managing anxiety and fear: Providing age-appropriate explanations and reassurance can help alleviate anxiety in children.
- Postoperative pain management: Children may require special pain management strategies to ensure their comfort.
4. Anesthesia for Cataract Surgery in Elderly Patients:
This search focuses on the anesthetic considerations for older adults undergoing cataract surgery, including:
- Increased risk of complications: Elderly patients are more likely to have underlying health conditions, which can increase the risk of complications from anesthesia.
- Adjusting anesthetic doses: Older adults may require lower doses of anesthetic medications due to their slower metabolism and potential drug interactions.
- Managing co-morbidities: Careful management of existing medical conditions is crucial to ensure a safe and successful surgical experience.
5. Anesthesia for Cataract Surgery with Pre-existing Conditions:
This search explores the anesthetic challenges associated with patients who have pre-existing medical conditions, such as:
- Diabetes: Patients with diabetes may require special considerations regarding blood sugar control and anesthetic management.
- Heart disease: Patients with heart disease may need modifications to anesthetic protocols to minimize cardiovascular risk.
- Lung disease: Patients with lung disease may require supplemental oxygen or other respiratory support during and after surgery.
6. Anesthesia for Cataract Surgery with Multiple Eye Surgeries:
This search examines the anesthetic management for patients undergoing multiple eye surgeries, including:
- Planning for multiple procedures: Anesthesia plans should consider the overall surgical schedule and the potential for cumulative effects of anesthetic medications.
- Minimizing discomfort: Choosing anesthetic techniques that minimize pain and discomfort is crucial, as patients may have multiple eye procedures scheduled close together.
- Ensuring a smooth recovery: Effective pain management and postoperative care are essential for patients undergoing multiple eye surgeries.
7. Anesthesia for Cataract Surgery with Advanced Cataracts:
This search focuses on the anesthetic considerations for patients with advanced cataracts, including:
- Longer surgery times: Surgeries for advanced cataracts may take longer, requiring careful anesthetic management to ensure patient comfort and safety.
- Potential for increased complications: Patients with advanced cataracts may have more fragile eye structures, potentially increasing the risk of complications during surgery.
- Postoperative recovery: Effective pain management and postoperative care are crucial to ensure a smooth recovery for patients with advanced cataracts.
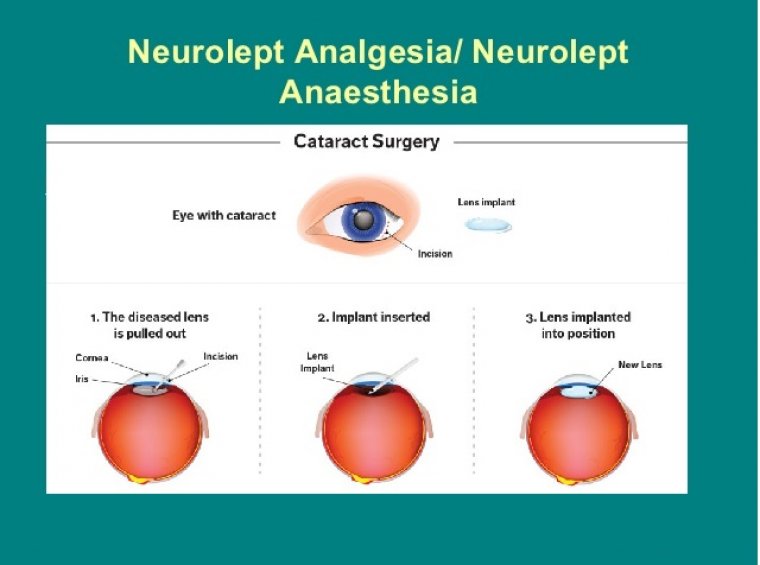
8. Anesthesia for Cataract Surgery with Lens Implantation:
This search explores the anesthetic aspects of cataract surgery with lens implantation, including:
- Choosing the appropriate anesthetic technique: The anesthetic technique should be tailored to the specific lens implant used and the overall surgical procedure.
- Minimizing intraoperative movement: The anesthetic should ensure complete immobility of the eye during lens implantation to prevent displacement or damage to the implant.
- Postoperative pain management: Patients who have undergone lens implantation may require additional pain management strategies to ensure a smooth recovery.
FAQs
Anesthesia for Cataract Surgery is a common procedure with many questions surrounding it. Here are answers to some frequently asked questions:
1. What is the most common type of anesthesia used for cataract surgery?
Topical anesthesia, involving the application of anesthetic drops to the eye, is the most commonly used anesthetic technique for cataract surgery. It is safe, effective, and generally well-tolerated by patients.
2. Is general anesthesia ever used for cataract surgery?
General anesthesia is typically reserved for complex cases, such as patients with significant medical conditions or those requiring additional procedures during cataract surgery.
3. How long does it take to recover from anesthesia for cataract surgery?
Recovery from topical anesthesia is usually very quick, with most patients able to resume normal activities within a few hours. Patients who have received general anesthesia or intravenous sedation may require a longer recovery period, typically a few days.
4. What are the potential side effects of anesthesia for cataract surgery?
The potential side effects of anesthesia for cataract surgery vary depending on the technique used. Topical anesthesia may cause temporary blurred vision or eye irritation. General anesthesia can lead to nausea, vomiting, or drowsiness. Regional anesthesia may cause pain, bleeding, or nerve damage.
5. Can I eat or drink before cataract surgery with anesthesia?
You will typically be instructed to fast for a certain period before cataract surgery, depending on the type of anesthesia you are receiving. This is to minimize the risk of complications during surgery.
6. What should I do if I have concerns about anesthesia for cataract surgery?
If you have any concerns about anesthesia for cataract surgery, be sure to discuss them with your ophthalmologist and anesthesiologist. They can provide you with personalized advice and address your specific questions.
7. Is it safe to have cataract surgery under anesthesia?
Cataract surgery is a remarkably safe procedure, and anesthesia plays a crucial role in ensuring its safety. However, as with any medical procedure, there are potential risks associated with anesthesia. It is essential to discuss your medical history and any concerns you may have with your doctor to ensure the safest possible anesthetic approach.
Tips for Choosing the Right Anesthesia for Cataract Surgery
Choosing the right anesthetic approach for cataract surgery is crucial for a successful and comfortable experience. Here are some tips to help you make an informed decision:
- Discuss your concerns with your ophthalmologist and anesthesiologist: Open communication with your healthcare providers is essential to ensure that your anesthetic needs are fully understood and addressed.
- Ask about the different anesthesia options: Learn about the different types of anesthesia available for cataract surgery, their benefits and risks, and which technique is most suitable for you.
- Consider your medical history: Share your medical history, including any allergies, medications, or pre-existing conditions, to help your doctors choose the safest and most effective anesthetic approach.
- Ask about postoperative pain management: Inquire about pain management strategies after surgery to ensure a smooth and comfortable recovery.
Conclusion
Anesthesia for cataract surgery is a dynamic field, constantly evolving to enhance patient comfort, safety, and overall surgical experience. The trends discussed in this article highlight the ongoing pursuit of personalized, minimally invasive, and technologically advanced anesthetic approaches. As we look towards 2025 and beyond, we can expect further advancements in anesthesia for cataract surgery, ultimately contributing to better outcomes and a more positive experience for patients. By staying informed about the latest trends and engaging in open communication with healthcare providers, patients can make informed decisions about their anesthetic care, ensuring a safe and successful cataract surgery journey.



Closure
Thus, we hope this article has provided valuable insights into Anesthesia for Cataract Surgery: Recent Trends 2025. We hope you find this article informative and beneficial. See you in our next article!
